Cervical myofascitis is an inflammation of the muscles and fascia (connective tissue) of the neck. This can be due to sudden trauma (such as whiplash injury) or chronic stress or overuse. Unlike a single “pulled” muscle which improves with rest, myofascitis tends to persist and worsen. Chronic inflammation can lead to scarring. 
Many factors may contribute to the development of myofascial pain. Abnormal stresses on the muscles from sudden tension on shortened muscles, maintaining a static position for a long period of time especially in a cold environment are thought to be common causes of myofascial pain. Poor posture is also a common cause.
Signs and symptoms
Myofascitis is characterized by pain and tenderness in a specific muscular region. Although it can affect various locations in the body (e.g., low back, buttocks, legs and arms), it is probably most common in the region of the neck. Patients usually report poorly localized pain. They can also report sensory disturbances (tingling or localized numbness).
Palpation of the affected muscle group(s) typically reveals deep-seated nodules and/or taut bands of muscle. These areas are hyperirritable and are called “trigger points.” Palpation of these trigger points may produce a “jump” sign where the patient jumps from pain.
Neck range of motion may be restricted. Patients frequently complain of poorly localized neck pain. They may also complain of radiation of the pain into the arm. The pain frequently 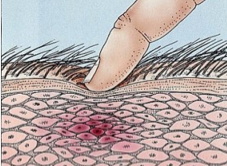 interferes with sleep.
interferes with sleep.
Cervical myofascitis can cause pain referred to the shoulder or arm, tightness, tenderness, popping and clicking, stiffness and limitation of movement and muscle weakness.
Treatment
Medications used in the treatment of cervical myofascitis include nonsteroidal anti-inflammatory drugs (e.g., ibuprofen), muscle relaxants, tricyclic antidepressants and anticonvulsants.
Physical therapy is used to stretch the tight muscle groups using massage, exercise and “spray-and-stretch” techniques. Trigger point injections with local anesthetic are and/or corticosteroids are used to “break up” the tension in these areas.
Additional modalities which can be useful in treatment include phonophoresis (the use of ultrasound to enhance the absorption of topically applied drugs), massage, stretching, electrical muscle stimulation, ultrasound, biofeedback and low-energy laser.
Osteopathic manipulation can help with release of muscle tension. Botulinum toxin type A can  also be injected into trigger points. Transdermal lidocaine patches are also helpful.
also be injected into trigger points. Transdermal lidocaine patches are also helpful.
Prevention of myofascial pain disorders rests on the use of properly designed ergonomic work stations. Patients should be encouraged to perform full range of motion of the cervical spine daily.
Recent studies evaluating the 18 tender points found in fibromyalgia patients have shown that trigger points in myofascial pain correspond to many of these sites leading to the hypothesis that active trigger points may lead to the development of fibromyalgia. In fact, in terms of differential diagnosis of myofascial pain, fibromyalgia should be excluded.






Leave A Comment