To understand plantar fasciitis it may help to first understand what the plantar fascia is. It is a band of thick fibrous connective tissue that runs from the calcaneus (heel bone) along the sole of the foot up to the toes and provides padding for your foot and support for the arch of the foot (Plantar Heel Pain 2014).
What is plantar fasciitis?
In medical terminology “itis” is indicative of a condition of inflammation; therefore plantar fasciitis is a condition of inflammation of the plantar fascia in the foot which may be accompanied by pain, structural deterioration, or fibrosis.
Who may suffer from plantar fasciitis? How do you get plantar fasciitis?
It is estimated that around one tenth of the population will suffer from plantar fasciitis at some point in life. The persons most likely to experience this condition are women, middle aged persons, the overweight, the elderly, runners, joggers, persons with “flat feet” (hyperpronation, which is a slight or non-existent arch), and persons that endure long periods of weight bearing (think of soldiers lugging around those 80 pound packs). Of these, the person with hyperpronation is the most likely to experience plantar fasciitis.
What are the symptoms of plantar fasciitis? How is plantar fasciitis diagnosed?
Symptoms of plantar fasciitis:
Tingling, numbness, swelling, and radiating pain are the most often complained symptoms. 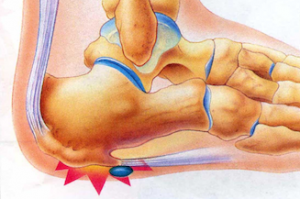 These are most likely to occur after prolonged periods of rest, usually sleeping but also sitting for long periods . When the person suffering plantar fasciitis wakes the pain is usually most severe when they first begin to walk after rising in the morning. The pain usually eases after having walked some (Considerations in footwear and orthotics 2014).
These are most likely to occur after prolonged periods of rest, usually sleeping but also sitting for long periods . When the person suffering plantar fasciitis wakes the pain is usually most severe when they first begin to walk after rising in the morning. The pain usually eases after having walked some (Considerations in footwear and orthotics 2014).
Other symptoms of plantar fasciitis are a decrease in the dorsiflexion of the foot which would indicate tightness or stiffness of the gastrocnemius muscle (back of the calves) or the Achilles tendon (at the back of the ankle).
This means that the muscles and tendons are stiff and lack flexion and so the toe of the foot has low flexibility and doesn’t point upward easily or at all. Stretching exercises performed on a step can help to stretch these muscles and tendons but be sure to consult with your physician before attempting any physical therapy or exercise program.
Diagnosis of plantar fasciitis:
Diagnosis of plantar fasciitis is performed by your physician first looking at the patient’s history and physical condition. Then your physician may perform certain tests to measure the flexibility of the gastrocnemius muscle and the Achilles tendon.
This physical examination will also look for tenderness and pain in the plantar fascia of the feet or the heels, as well as tenderness, tightness, and pain in the gastrocnemius muscle. Usually imaging tests such as x-ray or MRI are not necessary.
How is plantar fasciitis treated?
About 90% of the time plantar fasciitis will take care of itself within six months to a year with conservative treatment.
- Most often treatment with heat, ice, and rest combined with physical therapy will correct the condition (Plantar fasciitis: How best to treat? 2013). The physical therapy may
 consist of exercise for strengthening and stretching the gastrocnemius muscles and stretching the Achilles tendons. For persons that are overweight, losing weight to take the stress off of the foot is beneficial for recovery. NSAIDS such as aspirin or ibuprofen may be used temporarily to reduce inflammation.
consist of exercise for strengthening and stretching the gastrocnemius muscles and stretching the Achilles tendons. For persons that are overweight, losing weight to take the stress off of the foot is beneficial for recovery. NSAIDS such as aspirin or ibuprofen may be used temporarily to reduce inflammation. - In some cases corticosteroid injections may be used to relieve pain during therapy but there is risk involved. There are very slight risks of rupture of the plantar fascia, infection at the injection site, and plantar fat pad atrophy. For cases unresponsive to other nonsurgical procedures often PRP, stem cell injections or extracorporeal shockwave therapy may be used (Platelet-Rich Plasma Efficacy Versus Corticosteroid Injection Treatment for Chronic Severe Plantar Fasciitis 2014).
- Extracorporeal shockwave therapy (ESWT) is an outpatient procedure that usually takes about thirty minutes. It is a non-invasive procedure performed without anesthesia that utilizes electrotherapy directly on the plantar fascia (Low-Level Laser Therapy for the Treatment of Chronic Plantar Fasciitis: A Prospective Study 2014).
- Another non-surgical procedure that may be used in the treatment of plantar fasciitis is prescription pain creams, which is the application of customized creams onto the plantar fascia area.
Surgical Treatment of plantar fasciitis
However, if non-surgical forms of treatment fail it may be necessary to have a plantar fasciotomy, which is a surgical procedure that utilizes ultrasound to disrupt the fibrous tissue of  the plantar fascia intended to allow more area for the inflamed tissue. This procedure has some risks involved including injury of the nerve, infection, ruptured tissue, and failure to improve the condition.
the plantar fascia intended to allow more area for the inflamed tissue. This procedure has some risks involved including injury of the nerve, infection, ruptured tissue, and failure to improve the condition.
Some patients respond better to the treatments that others and you should discuss with your physician the best course of action for you. Surgery is necessary less than 5% of the time.






Leave A Comment